Lucy Tomlinson looks at the city's grim cancer statistics and asks what we can do about it
Manchester is a city particularly cursed when it comes to cancer.
One in two people will develop cancer at some point in their lives, according to the most accurate forecast to date from Cancer Research UK – that’s half of everyone born since 1960. So, if you are lucky enough not to get cancer yourself then the chances are a loved one will. That’s a parent or a wife, a husband or sibling, a friend or, god forbid, a child. It’s a sobering thought.
When it comes to the stats for Manchester, the news is even worse. The death toll from cancer is ten percent higher than the national average - in real terms this means around 6,500 people a year or eighteen people a day, according to 2014 figures.
Part of the reason for this is the higher smoking rates in Manchester, combined with the fact that the uptake of breast, cervical and bowel screening programmes (to prevent some cancers and detect others at an earlier, more curable stage) is significantly lower than the national average.
While it’s a supremely depressing thought that you are more likely to die from cancer if you live in Manchester than other parts of the country, there is hope. Manchester also has some of the best cancer resources in the country as well many dedicated researchers, clinicians and carers all working tirelessly to turn those stats around.

Manchester has been dubbed the ‘sick man of the UK’ and the ‘devomanc’ approach – integrating health and social care more tightly and therefore enabling decision-making to be carried out more responsively to the population it serves – is hoped to be able to get Manchester back to average health.
Greater Manchester Cancer is the cancer programme of Greater Manchester’s devolved health and social care system and in charge of marshalling a complex network of hospitals, universities, labs, charities in the fight against cancer. There are research specialisms galore, brought together under the aegis of The University of Manchester and Cancer Research UK which makes Manchester a world-leader in cancer research.
The Christie made many of the earliest advances in cancer care
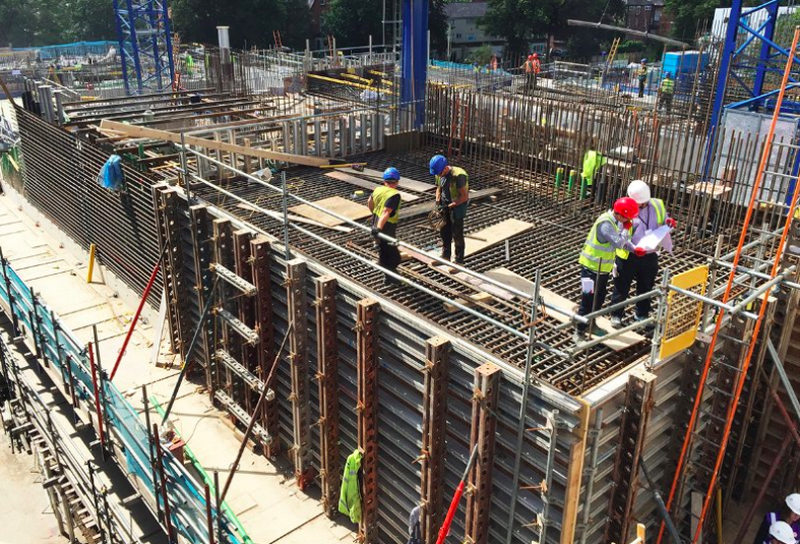
Some big names in this crusade include The Christie – one of only three specialist cancer centres in England – which is well known as one of the best cancer hospitals in the world (it was ranked in the top 10 most technologically advanced in the world). That is one of the reason’s its been chosen to house the UK’s first proton beam therapy centre (you may remember the case of Ashya King, whose cancer was apparently cured in this way) which is slated to open this August.
The Christie made many of the earliest advances in cancer care, from setting international standards in radium treatment in the 1930s (hence it becoming known as the ‘Manchester Method’), to the world’s first clinical use of Tamoxifen to treat breast cancer in the 70s to the original use of cultured bone marrow in the treatment of leukemia.
Such a sterling history means The Christie attracts funding and quality staff. Ran Mackay, Director of Physical Medicine, has just been awarded the NHS Healthcare Scientist of the Year, while it was recently announced that a consortium headed up by the hospital was awarded £6.8 million to investigate advanced therapies.
Meanwhile, a glitzier sort of fundraising was seen at The Principal this month at the annual Christie Ball, which raised £155,000 towards replacing equipment lost in the Paterson Building fire. The fire happened in April last year and severely affected research carried out there by The University of Manchester and Cancer Research UK.
The ball was also the opportunity for the Tim Bacon Foundation to announce that it will be donating £500,000 to The Christie. Tim was a huge name on the Manchester food scene and is still sadly missed by many.
The people in the foyer had the strain of the experience written all over their faces
Manchester is also committed to turning things around in the field of prevention. I went to see Professor Anthony Howell of the Genesis Prevention Centre at Wythenshawe. The Genesis Prevention Centre itself is a collaborative venture with the NHS, and is part of a larger group of top experts in a variety of different fields who have all come together with the intention of making breast cancer a preventable disease.
The tension in the waiting room was high. The people in the foyer had the strain of the experience written all over their faces. But the appointment with Professor Howell could not have been more lighthearted – it felt like a jolly chat rather than a detailed examination of my medical and genetic history. Using that most sophisticated of medical equipment - a pencil and paper – he took me through all the risk factors for a woman of my age and found I was at a higher risk than average of developing breast cancer.
He then counselled me on what to do to keep my risk to a minimum, all standard advice such as eating well, keeping weight down and exercising, but hearing it from a world-class expert in cancer prevention somehow made it more real than reading a leaflet. I immediately mentally committed to radically overhauling my lifestyle. If I’m as healthy and chipper in my 70s as Professor Howell is, I will be a very happy woman.
While the commitment to prevention is obviously the first line of defence, recently much more thought has been put into the emotional and psychological wellbeing of patients while they go through treatment. The Maggie’s Centre is a marvel of lightness and calm, a retreat from the intensity and efficiency of The Christie. As the head of the centre, Sinead Collins, said to Confidential, ‘people need more then medicine.’
Laura, a local mum of two boys, was kind enough to share her experience of Maggie’s:
“I actually, strangely, looked forward to going across the road to Maggie's Centre with either my mum or husband. It's almost hard to put into words but I felt all the noise and bustle of everything surrounding cancer stopped when I walked through their doors. They were there if I needed them and always welcoming around the tea area for a chat.
"It's actually made me quite emotional looking at that photo as I'm so grateful for the centre for just being there. I was there mainly over the summer and I loved the garden where they grow their own fruit and veg for making soups and salads in the kitchen. It was very quiet and still which is just what's needed after everything across the road.”
Happily, Laura has finished treatment and is doing well. However, the top-class resources that the people of Manchester have come to rely on are not immune to the worries of the world. A vast amount of the cancer research is done by the Faculty of Biology, Medicine and Health at the University of Manchester, which is slated to lose 65 academic jobs with a further 627 at risk, in the recently announced cuts. Many commentators have blamed this on the financial uncertainty caused by Brexit.

And it is also essential to note that all these wonderful prevention programmes and centres of excellence balance precariously on top of the foundation of all healthcare – the relationship between a patient and his or her doctor. The first and best diagnostic tool is a real life human being and there is a worrying trend. According to a report by the Kings Fund, the quality of the GP-patient relationship is critical in identifying cancer sooner, with early identification being the most important factor in patient survival.
But one potential problem for cancer outcomes is the proposal to combine GP practices. In practice this means successful surgeries absorbing struggling ones in order to bring them up to standard. The upshot being that if your GP practice was responsible for 5,000 patients it might become responsible for 10,000 patients and although the patient/GP ratio might remain roughly the same, the chances of you seeing the same doctor successively drop. Now, we are all familiar with the complaint that you never get to see the same doctor and this doesn’t look like resolving anytime soon, so the best advice is to become your own advocate. Record symptoms, keep up to date with checks and get to know your own body.
Set against this are new approaches to diagnosis which aim to get patients into the system more quickly than ever. The North West Lung Centre at Wythenshawe (another top-class facility) has launched the RAPID Programme to dramatically reduce the time taken to complete investigations in patients where there is any suspicion of lung cancer. The aim is to ensure all patients have a clear diagnosis, whether that is lung cancer or not, within seven days of referral.

The final and possibly most innovative weapon in the fight against cancer is each other, harnessing the power of our social networks to raise awareness of the most prevalent kinds of cancer. Based on the idea that we are much more likely to listen to one another than a leaflet, this citizen-led social movement includes the development of a network of 20,000 cancer champions to spread awareness in their local community. A similar idea is being rolled out to reduce smoking.
Cancer is depressing. It is scary. It will touch most of our lives. And despite the fighting talk it can’t be beaten in all cases. But as a city we desperately need to improve our odds. It’s not just up to those clever people in the labs, but to all of us.
Cancer prevention – what can you do?
First of all – stop smoking!
The usual advice: less drinking, more exercise, a better diet with more fruit and veg. Do it.
Attend the appropriate screenings for your demographic.
Keep an eye on friends and loved ones – urge people to get their GP if they suddenly lose weight, complain of feeling tired or develop a persistent cough
Lastly STOP SMOKING.
You can become a Cancer Champion by signing up here.